Cancer treatment planning is a complex and crucial process that involves selecting the most appropriate therapies to target cancer cells while minimizing side effects and maximizing patient outcomes. Empowering patients and healthcare professionals with the necessary insights for effective treatment planning is essential in the fight against cancer. This blog post explores the key considerations, strategies, and insights into cancer treatment planning, aiming to support informed decision-making, personalized care approaches, and optimal treatment outcomes for individuals battling cancer.
Understanding the Importance of Cancer Treatment Planning
Cancer treatment planning is a comprehensive and individualized approach that considers various factors, including cancer type, stage, location, genetic profile, overall health, treatment goals, and patient preferences. A well-structured treatment plan guides healthcare providers in determining the most suitable treatment modalities, such as surgery, chemotherapy, radiation therapy, immunotherapy, targeted therapy, or a combination of treatments, to achieve the best possible outcomes for each patient. Effective treatment planning not only targets cancer cells but also addresses symptom management, supportive care needs, quality of life considerations, and long-term survivorship goals, emphasizing holistic care and patient-centered decision-making throughout the treatment journey.
Key Elements of Cancer Treatment Planning Insights
Multidisciplinary Approach
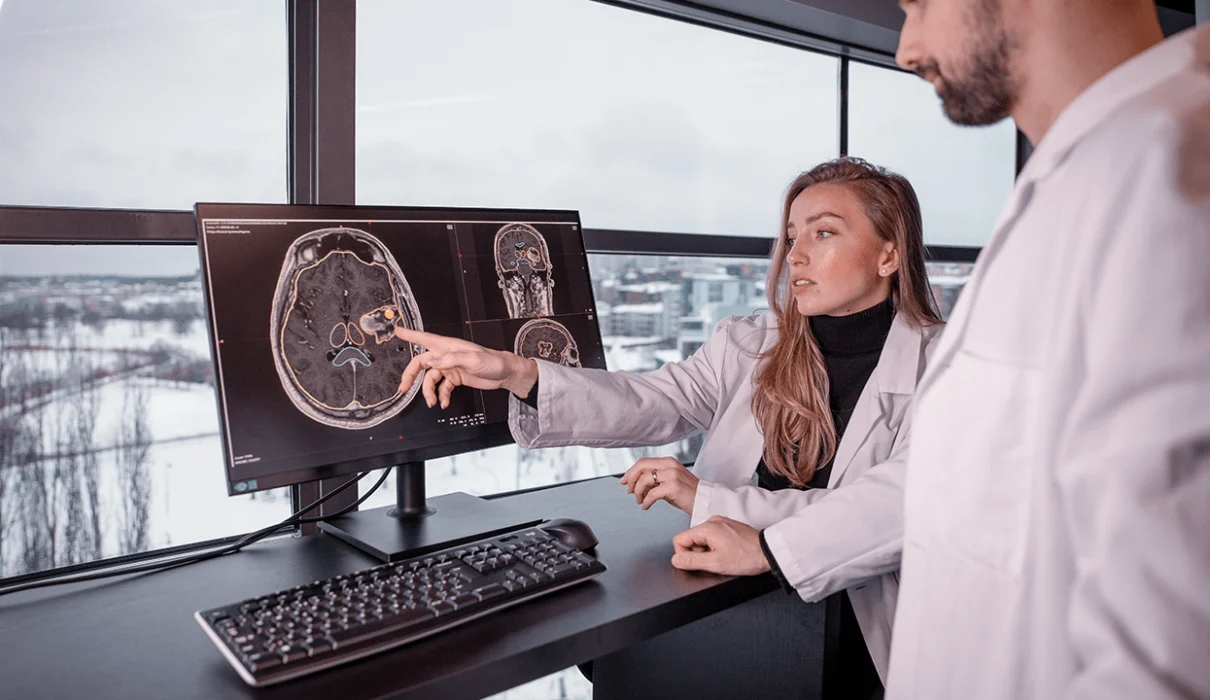
A multidisciplinary approach to cancer treatment planning involves collaboration among oncologists, surgeons, radiation oncologists, pathologists, radiologists, nurses, social workers, and other healthcare professionals to develop comprehensive treatment plans tailored to each patient’s unique needs. Multidisciplinary tumor boards, cancer conferences, and collaborative care models facilitate communication, shared decision-making, and consensus on treatment recommendations, ensuring that patients receive coordinated, evidence-based care from a diverse team of experts, optimizing treatment outcomes and quality of care delivery.
Personalized Treatment Strategies
Personalizing cancer treatment strategies based on individual characteristics, tumor biology, genetic markers, and treatment responses enhances treatment effectiveness and minimizes potential side effects. Precision medicine approaches, such as molecular profiling, genetic testing, and biomarker analysis, help identify targeted therapies, immunotherapies, or clinical trials that may offer optimal responses for specific cancer subtypes, guiding treatment selection, monitoring treatment efficacy, and adapting therapies based on real-time data, promoting personalized care, treatment innovation, and improved outcomes in cancer treatment planning.
Shared Decision-Making and Informed Consent
Shared decision-making between patients and healthcare providers is essential in cancer treatment planning, empowering patients to actively participate in treatment decisions, express preferences, and make informed choices about their care. Healthcare professionals should engage patients in discussions about treatment options, risks, benefits, and expected outcomes, provide educational resources, and obtain informed consent before initiating treatments, fostering trust, transparency, and collaboration in the decision-making process, ensuring that treatment plans align with patient values, goals, and preferences, enhancing patient satisfaction and treatment adherence throughout the cancer care continuum.
Strategies for Empowering Cancer Treatment Choices
Psychosocial Support and Counseling
Offering psychosocial support, counseling services, and mental health resources to patients and families helps address emotional distress, anxiety, depression, and coping challenges associated with cancer diagnosis and treatment. Psychosocial interventions, support groups, mindfulness programs, and counseling sessions promote emotional well-being, resilience, and adaptive coping strategies, reducing psychological distress, improving quality of life, and enhancing patient resilience and mental health during cancer treatment and survivorship, promoting holistic care and wellness for individuals affected by cancer.
Integrating Mental Health EMR Systems in Cancer Care
Integrating Electronic Medical Records (EMR) for mental health into cancer care marks a major step forward in comprehensive patient management. This approach enables smooth tracking and management of the psychological aspects of cancer treatment, ensuring mental health is a key part of care planning. Mental health EMR systems streamline the recording of psychological assessments, treatments, patient progress, and team communication, considering all aspects of the patient’s health. These systems improve understanding of the patient’s mental health, enhancing care plans to swiftly identify and address mental health issues like depression, anxiety, and stress. This not only affects treatment success but also improves the quality of life for cancer patients.
Advocacy and Patient Navigation
Engaging patient advocates, navigators, and support networks can help patients access resources, overcome barriers to care, and advocate for their healthcare needs in cancer treatment planning. Patient navigators, advocacy organizations, and peer support groups can provide guidance, emotional support, and practical assistance to patients navigating complex treatment decisions, financial challenges, and healthcare system barriers, empowering patients to navigate the cancer care continuum more effectively, promoting patient-centered care and health equity in cancer treatment planning.
Cancer treatment planning is a complex process that requires collaboration, personalized approaches, shared decision-making, and ongoing support to achieve optimal outcomes for patients. By incorporating key elements such as multidisciplinary teamwork, survivorship planning, patient education and empowerment, psychosocial support, and patient advocacy into cancer treatment plans, healthcare professionals can improve treatment outcomes, enhance patient satisfaction and quality of life, and promote holistic care for individuals affected by cancer. With ongoing advancements in precision medicine, technology, and patient-centered care models, the future of cancer treatment planning holds even greater potential for optimizing treatments, minimizing side effects, and promoting overall well-being for cancer patients.